CarrotCube works as a booster dose for the delivery of Next-Gen Healthcare
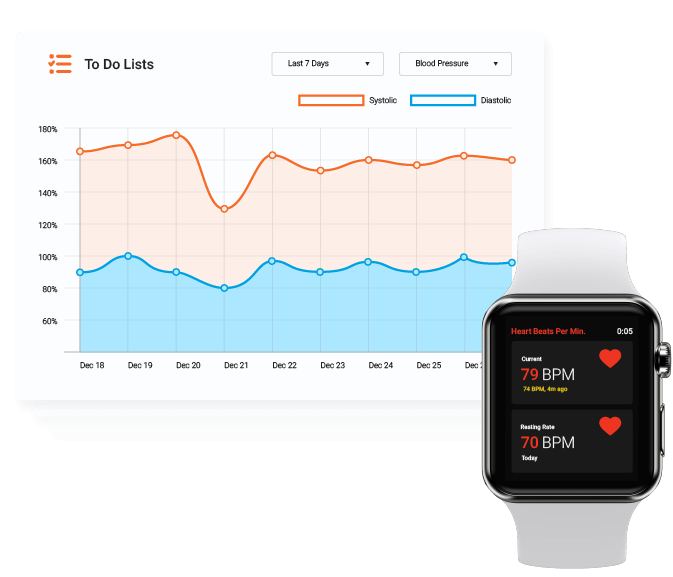
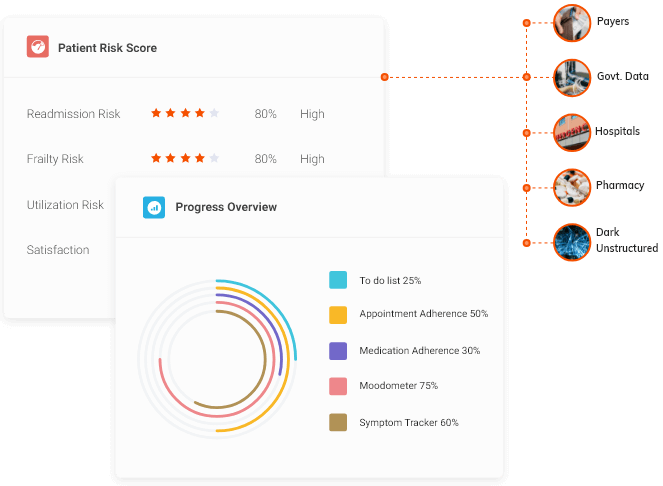
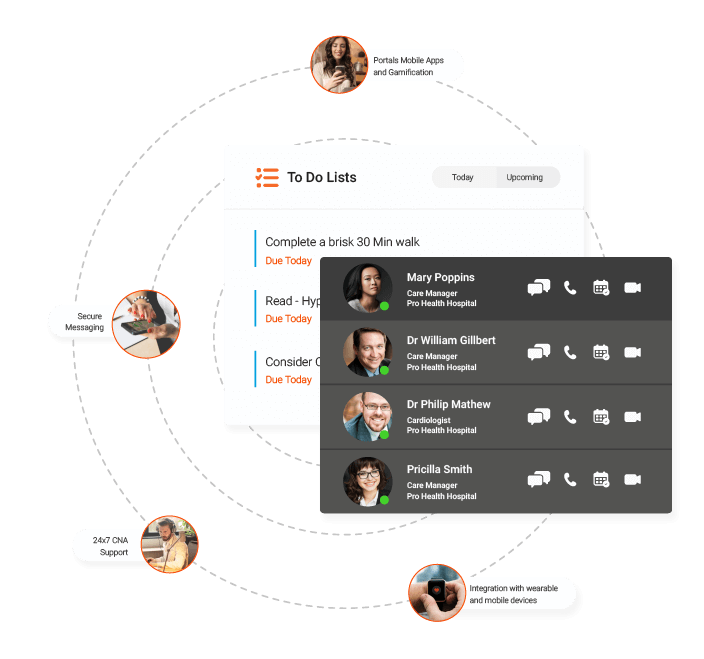
CarrotCube seamlessly integrates clinical workflows to manage patient health more efficiently. Built on Salesforce Health Cloud, it provides a 360° view of the patient's’ medical profile, making continuous care delivery and collaboration possible from the time a patient walks into the hospital and throughout the continuum of care.
Result, value-based care models, with value based reimbursements, significantly lower readmission rates, more savings on administrative costs and a marked improvement in preventive care initiatives, making it a win-win for both providers and patients.

 Play Video
Play Video





 Schedule a Demo
Schedule a Demo











 Apr 2020
Apr 2020 3 Minutes Read
3 Minutes Read
 Read More Blogs
Read More Blogs










